Managing hypertension will change more in next 5 years than the last 100 years
Managing hypertension will change more in next 5 years than the last 100 years. That’s a bold statement, so I’d like to explain why we at Valencell believe it and how we’re seeing it play out in real time.
Wearables & medical devices are rapidly converging
We’ve said this many times before and the trend continues. In fact, its accelerating particularly as the COVID-19 pandemic has highlighted the health & medical capabilities of wearable devices.
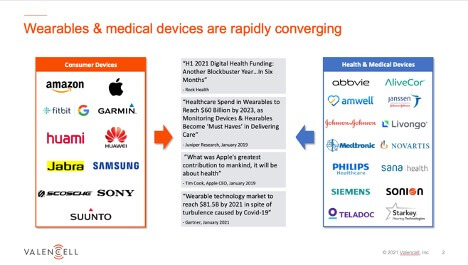
Nearly all the consumer wearables companies are moving toward becoming at least personal health devices, and in some cases regulatory cleared medical devices. Health and medical device companies are also joining the movement in creating and/or using devices intended to be worn outside of medical facilities. This involves a wide range of “health & medical” companies, including traditional medical device companies, startup med device companies, pharma, clinical research, hearing health, digital therapeutics, remote patient monitoring, and many more.
Foundation is set to unlock large scale value creation
The history of wearable devices can be broken into three generations going back to around 2010.
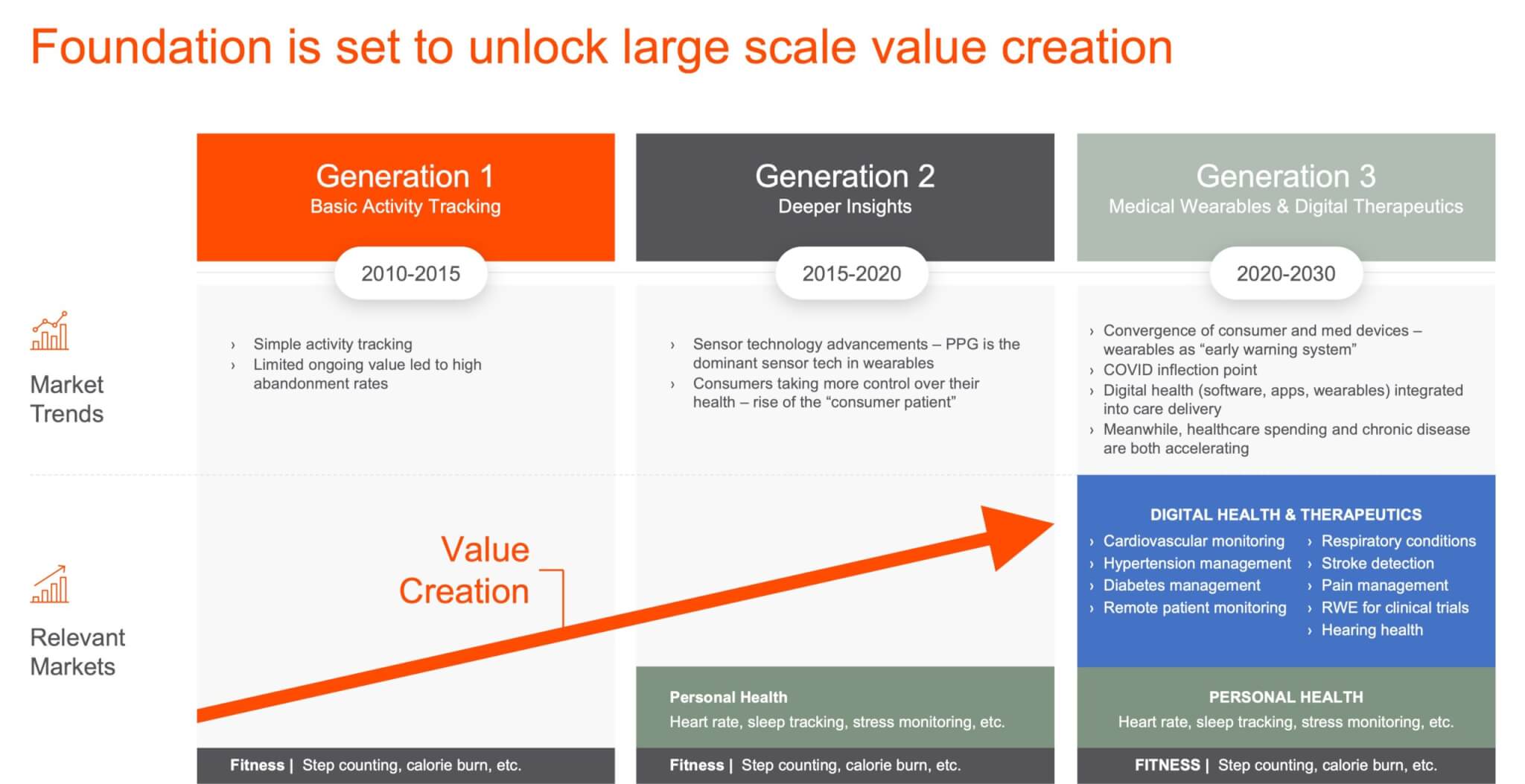
Generation 1 – Basic activity tracking
Generation 1 was highlighted by basic activity tracking, typically using accelerometers in simple wearable devices. Think first generation Fitbits, Nike Fuel Bands, or Jawbone wristbands. These devices were useful in helping people understand how much they were moving and basic activity levels. However, limited ongoing value led to high abandonment rates.
Generation 2 – Deeper insights via biometric sensors
Around 2015 biometric sensors were being added to wearable devices at scale. PPG sensors would become the dominant sensor modality in wearable devices because of the accuracy, flexibility to implement in different device types, and multiple biometrics that can be measured with PPG. This is when the convergence of consumer wearables and health/medical devices began, and when wearables sharpened their focus on being personal health devices.
Generation 3 – Medical wearables & digital therapeutics
Second generation wearables set the stage for the third generation of wearables, which is highlighted by the move toward proactive monitoring, predictive modeling and the emergence of consumer medical wearables being used to impact patient outcomes. This is happening in screening, diagnostics, and therapeutics across numerous health conditions and patient workflows.
The third generation of wearables is unlocking value in numerous areas across health and medical use cases. So why the focus on hypertension? You could argue many of these chronic diseases are ripe for change, but most are making more progress than hypertension. For example, in cardiovascular conditions you have heart rate monitors now ubiquitous in wearables and now can detect arrythmias and atrial fibrillation with medical-grade accuracy from companies like AliveCor. In respiratory conditions, we’ve seen decades of smoking cessation efforts finally having an impact, along new innovations in digital health from companies like Propeller Health and Resmed. In diabetes management, you have continuous glucose monitors becoming more common and companies like Virta Health proving that type-2 diabetes is indeed reversible.
Managing hypertension by comparison has lagged.
Hypertension is a massive global public problem
We now have over 1 billion people with high blood pressure worldwide, accounting for more than 10 million deaths per year. Patient treatment protocols simply have not kept up.

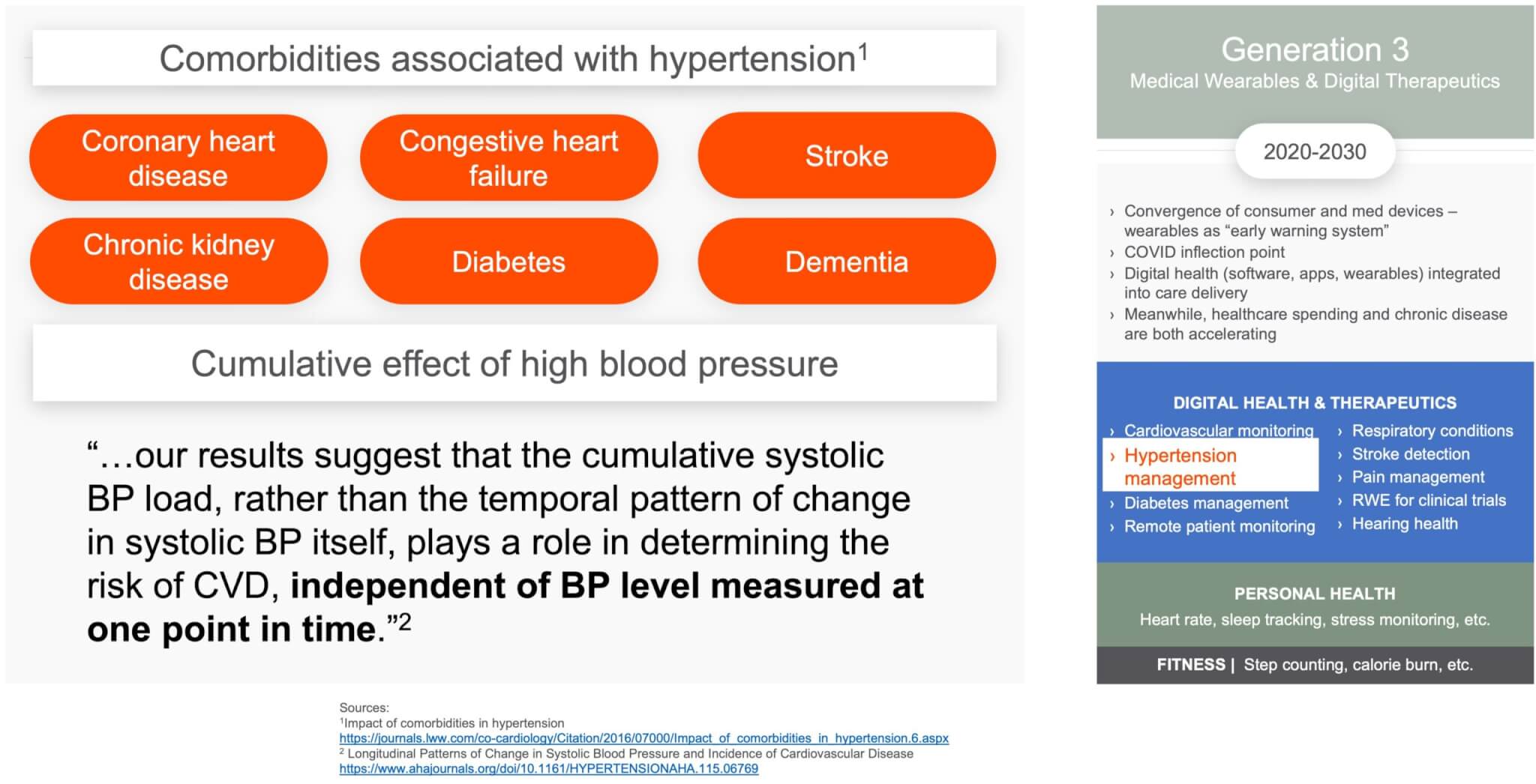
Hypertension comorbidities & cumulative high blood pressure multiply the impact
As if that’s not enough, the comorbidities associated with hypertension and the cumulative effect of high blood pressure multiply the impact of the condition. The cumulative effect of high BP that accelerates the damage caused by high blood pressure, combined with the fact that it has no outward symptoms (why they call it the “silent killer”), makes the frequency and ease of BP monitoring extremely important to enable early interventions.
But there is reason for hope. We believe we’re at an inflection point that is dramatically changing hypertension management forever.
Managing hypertension will change more in next 5 years than the last 100 years
Yes, it’s a bold statement, but here’s why it’s entirely possible, even probable.
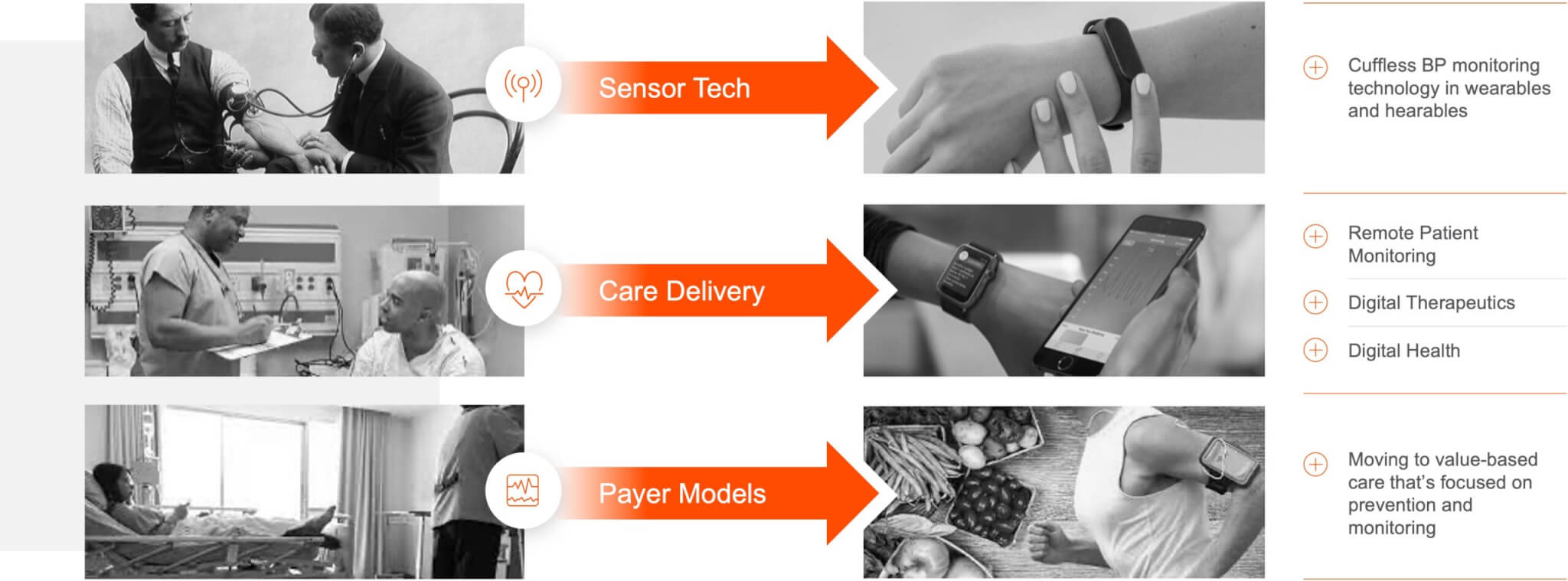
- Sensor tech – There’s been no meaningful innovation in BP sensors in over 100 years. The blood pressure cuffs used today are eerily similar to those first introduced in the market in the early 1900’s. That’s changing now with wearable, cuffless BP technology being approved by regulatory bodies and being deployed in the field.
- Care delivery – Healthcare delivery is moving out of the hospital, into the home and everyday life. You can see this in the growth of remote patient monitoring, digital therapeutics, and digital health more broadly in the last few years. COVID-19 has certainly been an accelerant for this, but we’re still in the early stages of this play out.
- Payer models – Payer models are moving from fee-for-service to value-based care, which means among other things a shift in focus toward prevention and monitoring. This is moving slowly but showing real signs of progress.
And we’ve seen this movie before…
Sensor Tech: We’ve seen this play out before
Looking back on the first generation of wearables, if you wanted to measure heart rate the only viable method was with an ECG chest strap. At their peak, chest straps sold around 20 million units annually. There are now hundreds of millions heart rate monitors embedded in wearable devices around the world, with that number expected to reach over 1 billion by 2025. These devices how also support a variety of other measurements beyond heart rate, including heart rate variability, pulse oximetry, skin temperature and much more.
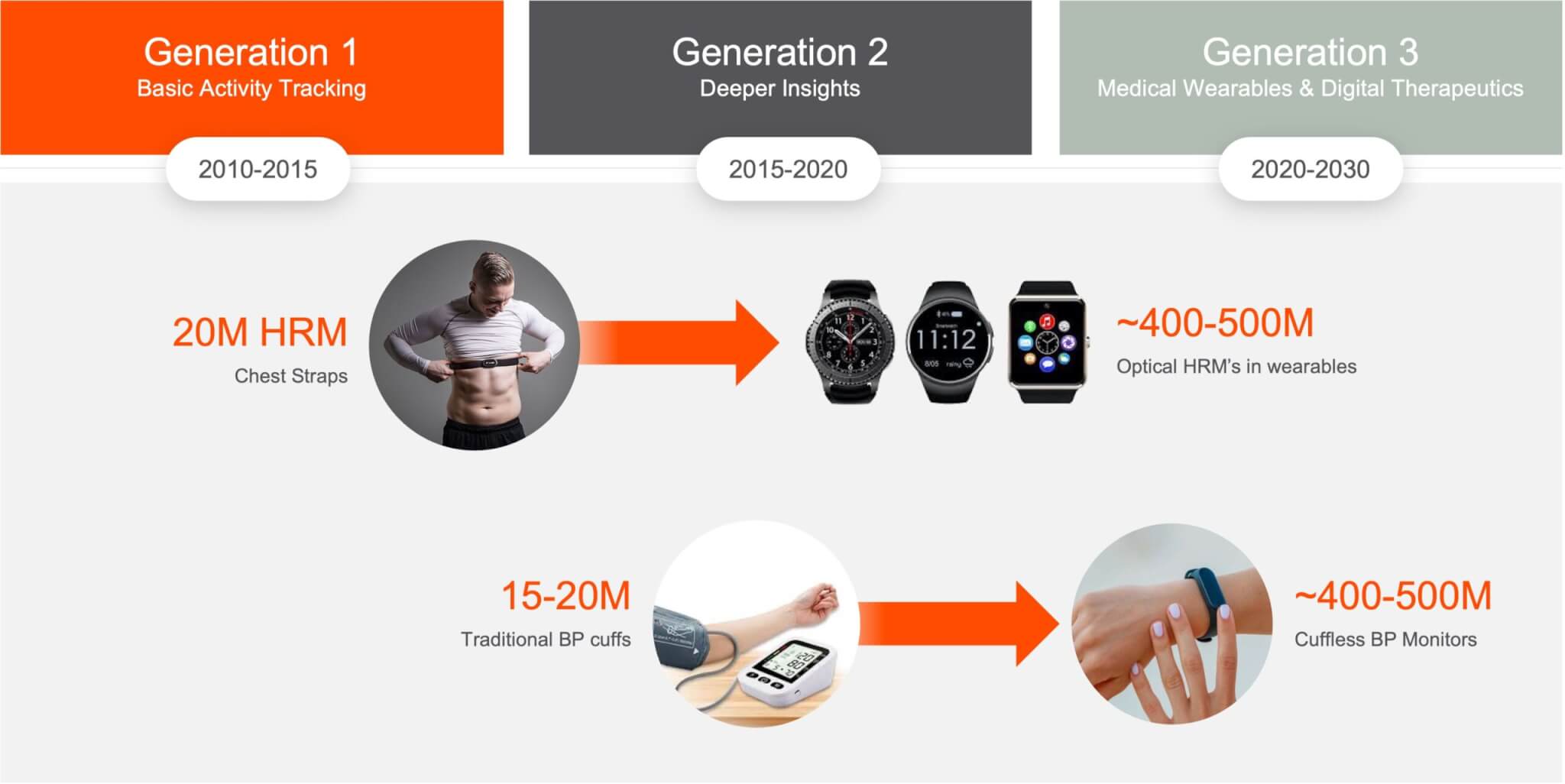
Blood pressure monitoring will take the same trajectory but will make a bigger impact on individual and public health because with blood pressure the metric is the use case. You don’t have to explain why a blood pressure reading is valuable, in the ways that were required in the early days of heart rate monitoring. In addition, wearable adoption is much larger at this point and the blood pressure market is more valuable and impactful (see comorbidities above).
Care Delivery: Moving outside the healthcare facility
Care delivery is indeed moving out of the hospital, into the home and people’s everyday lives. One way you can see this is in the massive growth of remote patient monitoring, digital therapeutics, and digital health across the industry. For example, McKinsey is standing by its estimate that up to $250 billion of current US healthcare spend could potentially be virtualized. In addition, digital health funding is setting records nearly every month or quarter. Rock Health reported the first half of 2021 saw $14.7B in digital health funding, already surpassing all of 2020’s funding – which was already a record year.

More importantly, we’re now starting to see clinical research studies demonstrating digital health solutions and digital therapeutics having an impact on hypertension management and other chronic diseases.
Payer Models: Moving to Value-Based Care
Payer models are moving from fee-for-service to value-based care, slowly but surely. This means among other things a shift in focus toward prevention and monitoring, particularly around chronic diseases which are the major burdens of disease today. Specific to hypertension, you are beginning to see reimbursement codes get approved for remote monitoring of high blood pressure. Beginning Jan. 1, 2020, US physician practices that educate patients to perform BP self-measurement can submit claims using CPT codes associated with clinical services.
- CPT 99473 – Self-measured blood pressure using a device validated for clinical accuracy; patient education/training and device calibration
- CPT 99474 – Separate self-measurements of two readings one minute apart, twice daily over a 30-day period (minimum of 12 readings), collection of data reported by the patient and/or caregiver to the physician or other qualified health care professional, with report of average systolic and diastolic pressures and subsequent communication of a treatment plan to the patient
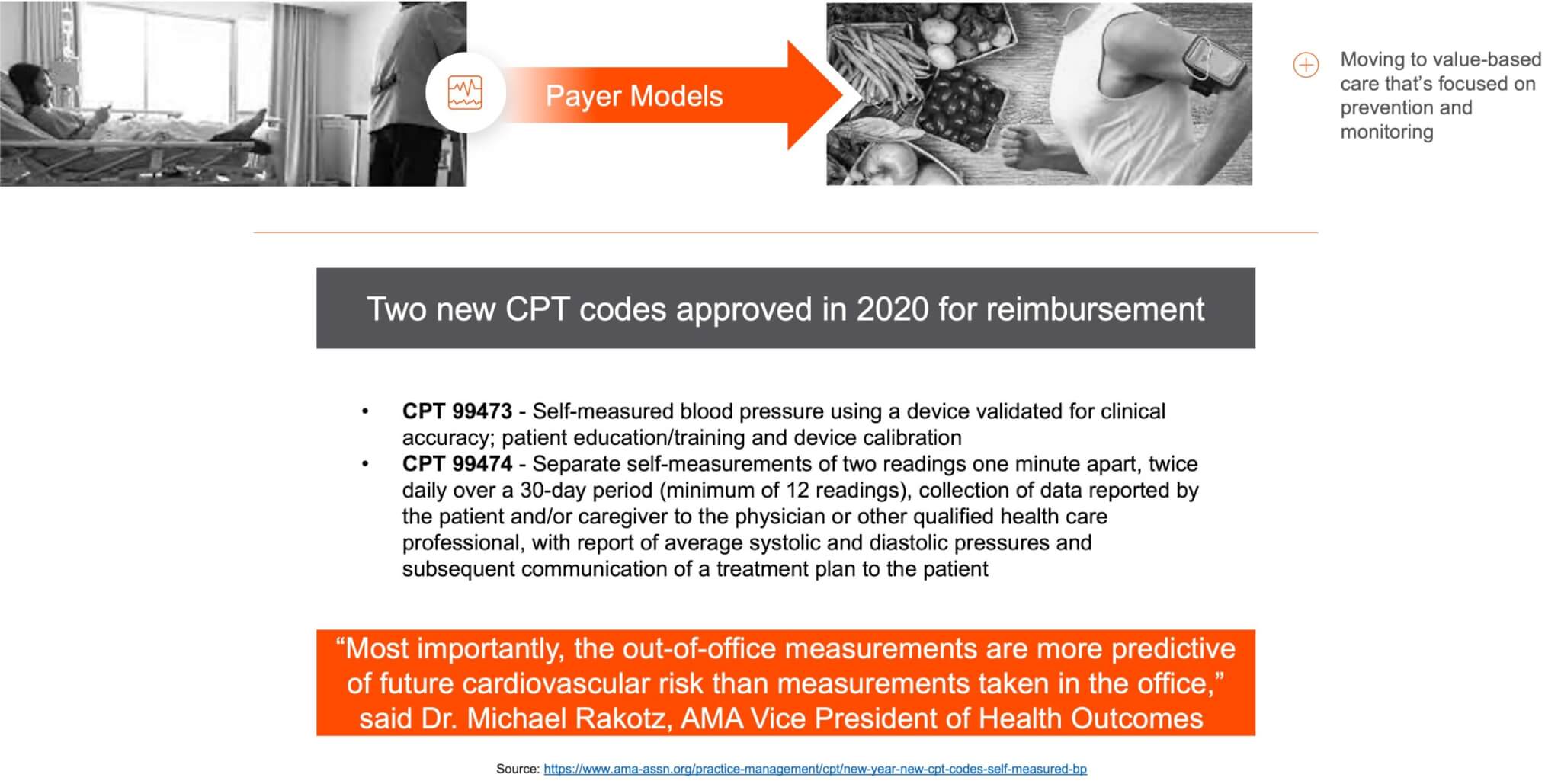
The AMA describes this as a recognition that more frequent measurements outside medical facilities are more insightful and predictive, and help address situations of white coat syndrome and/or masked hypertension.
Huge opportunity to impact patient outcomes and public health costs
According to the CDC, hypertension is one of the costliest health conditions in the US, associated with over $79 billion in total annual medical costs.
This presents a massive opportunity to impact patient outcomes and public health costs. There is more than enough incentive at the individual, company, and system levels for change to happen, and happen fast (by healthcare industry standards).