What is cumulative blood pressure and why does it matter?
Increasing amounts of clinical research are pointing to the importance of so-called “cumulative blood pressure” calculations, as opposed to measurements from a single day or period of time, in assessing risk for a long list of health conditions ranging from cardiovascular disease (CVD) and stroke to dementia, cognitive performance, and kidney damage. Researchers have begun to demonstrate that the more the human body is exposed to high blood pressure, both in duration and magnitude, the more direct and indirect damage is caused. This post will dive into the latest research and the implications for managing hypertension going forward.
What is cumulative blood pressure?
Cumulative blood pressure simply refers to your total “dose” of blood pressure over time. For example, a brief jump or drop in blood pressure is not likely to affect one’s cumulative blood pressure, but continuously elevated blood pressure over a significant period of time would play a major role in one’s mortality risk.
Mathematically, cumulative exposure is generally calculated as the product of the dose level and the exposure time and has been used to predict the impact of exposures on the human body. So, to measure cumulative blood pressure most studies sum the product of average millimeters of mercury and the years between each measurement over the years of follow-up in the study. For example, one study defined cumulative blood pressure levels as follows:
Cumulative blood pressure (cumBP) was calculated as described by Zemaitis et al.10. cumBP = [(BP1 + BP2)/2 × time1–2] + [(BP2 + BP3)/2 × time2–3], where BP1, BP2, and BP3 were measurements of BP recorded from the first, the second, and the third medical examination; time1-2 and time2-3 were the time intervals between the first and the second, and the second and the third BP measurements.
Source: https://www.nature.com/articles/srep41969
It is interesting to note that most of these studies measured blood pressure once every few years at best and still demonstrated results. Some had measurement gaps of 5-10 years!
Here’s an example:
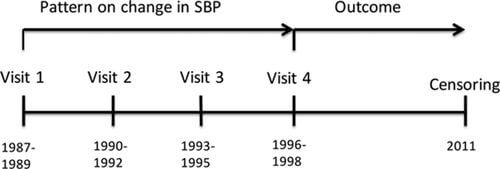
Imagine if this research had several readings per day or week! We’ll come back to that.
What does the latest research on cumulative blood pressure show?
An increasing amount of clinical research is showing that cumulative exposure to even moderate elevation of BP is independently associated with increased future cardiovascular risk, as well as risk for numerous other debilitating conditions. For example, exposure to higher BP levels from young to midlife is associated with worse gait and cognitive performance in midlife, which have been shown to be precursors to dementia even at BP levels below the clinical definition of hypertension. In addition, nocturnal cumulative systolic blood pressure and cumulative pulse pressure load (the area between the SBP curve and the DBP curve), relative to mean blood pressure, were superior in predicting hypertensive target organ damage.
Here’s a quick look at some of the research:
In this long-term cohort study, we demonstrated that elevated cumulative BP level was significantly associated with increased risk of CVD, and that this association was independent of BP measurements at one examination. These findings emphasize the importance of 10-year cumulative systolic BP as a risk factor to CVD, above and beyond current systolic BP.
Predictive Value of Cumulative Blood Pressure for All-Cause Mortality and Cardiovascular Events
In the current analysis, we found that for the study population, the cumulative incidence of all-cause mortality, CCEs (cardiovascular and cerebrovascular events), MI (myocardial infarction), and stroke increased with the increase in cumulative systolic BP (P < 0.05). cumSBP and cumDBP had better predictive value for endpoint events than baseline SBP and DBP using the same models, since cumulative exposure has evaluated the effect of exposure time as well as the exposure level, and is therefore a better predictor for the chronic effects of exposure on the target organs. However, there were some limitations to this analysis, since the mean follow-up was < 4 years, which was relatively short, so that some of the endpoint events might not have sufficient time to develop.
The cumulative blood pressure load and target organ damage in patients with essential hypertension
The cumulative blood pressure load is a better indicator of blood pressure consequences, and the nocturnal cumulative systolic blood pressure and cumulative pulse pressure loads could predict target organ damage. The cumulative pulse pressure load (cPPL) was defined as the area between the SBP curve and the DBP curve, which reflected the magnitudes and durations of the fluctuations in the cardiac cycles
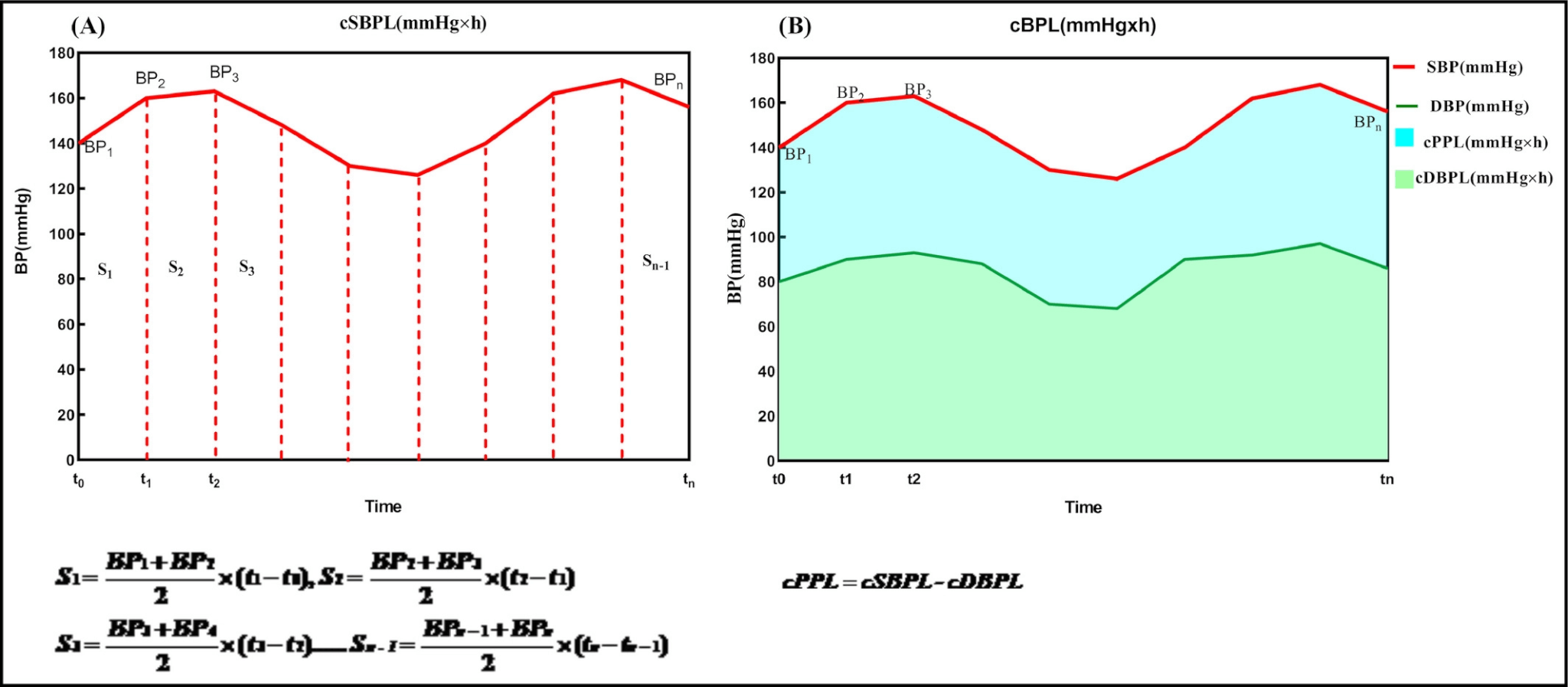
These results suggest that the cSBPL (cumulative systolic BP) and cPPL (cumulative pulse pressure load) can specifically predict hypertensive TOD (target organ damage – TOD was defined as the presence of left ventricular hypertrophy (LVH) and/or carotid and/or renal function impaired) and that particular attention should be given to the magnitudes and durations of nocturnal BP fluctuations when managing patients with hypertension.
Cumulative exposure to higher blood pressures from young adulthood to midlife, even at levels below the clinical definition of hypertension, associates with worse gait and cognitive function in midlife. The impact of cumulative levels of blood pressure exposure was independent of other vascular risk factors during a follow-up period of 30 years. Higher burden of midlife cerebral white matter hyperintensity on magnetic resonance imaging moderates the association of cumulative blood pressure exposure with gait, but not with cognitive function. The deleterious effect of elevated blood pressure on brain structure and function may begin during early adulthood, emphasizing the need for primordial prevention of high blood pressure, but also reconsidering individual levels of blood pressure for diagnosis of hypertension.
Hypertension disrupts the structure and function of cerebral blood vessels, leads to ischemic damage of white matter regions critical for cognitive function, and may promote Alzheimer pathology. There is strong evidence of a deleterious influence of midlife hypertension on late-life cognitive function, but the cognitive impact of late-life hypertension is less clear. Observational studies demonstrated a cumulative effect of hypertension on cerebrovascular damage, but evidence from clinical trials that antihypertensive treatment improves cognition is not conclusive.
What are the implications of this cumulative blood pressure research?
When considering the implications of cumulative blood pressure, it’s important to keep in mind the well-documented impact that lowering blood pressure can have on mortality and many diseases. Large meta-analyses have shown that for very 10 mm Hg reduction in systolic blood pressure significantly reduced the risk of major cardiovascular disease events, coronary heart disease, stroke, and heart failure, which led to a significant 13% reduction in all-cause mortality.
In addition, according to the CDC, “improvements in high blood pressure control or further reductions in the number of people with high blood pressure could generate billions in health care cost savings every year.”
So, what are the implications of cumulative blood pressure?
- First, the research demonstrates the need for regular BP monitoring over many years, even before elevated BP levels begin to present. As one study pointed out:
“The deleterious effect of elevated blood pressure on brain structure and function may begin during early adulthood, emphasizing the need for primordial prevention of high blood pressure, but also reconsidering individual levels of blood pressure for diagnosis of hypertension.”
- Second, the studies highlight the need to make BP monitoring much simpler and more convenient for patients as they go about their daily activities. The term “simpler” is particularly important in this context, as current commercial efforts of reducing the cuff burden of BP monitoring via cuffless technology have also come with painful calibration and recalibration steps, which arguably defeat the purpose.
- Lastly, these studies also highlight the need for more research will more granular data collection to understand not only cumulative BP in more detail, but also the impact of BP variability on clinical outcomes.
The data collection in these studies speaks to the challenge of monitoring outcomes in clinical studies on chronic diseases more broadly, but also highlights the opportunity to use modern technologies (like cuff-less, calibration-free BP monitoring) and remote patient monitoring to dramatically increase the ease and frequency of measuring BP. Similar to how the emergence of continuous glucose monitors (CGM’s) has demonstrated the importance of glycemic variability, there is good reason to believe BP variability is an important metric to monitor in the future.
Consumer medical wearables provide a platform to accomplish both simplicity/convenience and accurate BP readings over long timeframes. More specifically, cuff-less calibration-free BP monitoring will enable clinical and economic studies to further explore the impact of cumulative BP in the field. We look forward to contributing to those studies in the future.